Dealing with COVID-19 in Jewish nursing homes
As America’s battle with the novel coronavirus raged, no age group has been as widely affected as the elderly, making nursing homes, assisted-living facilities and senior residences ground zero in the battle against the virus, at least at first.
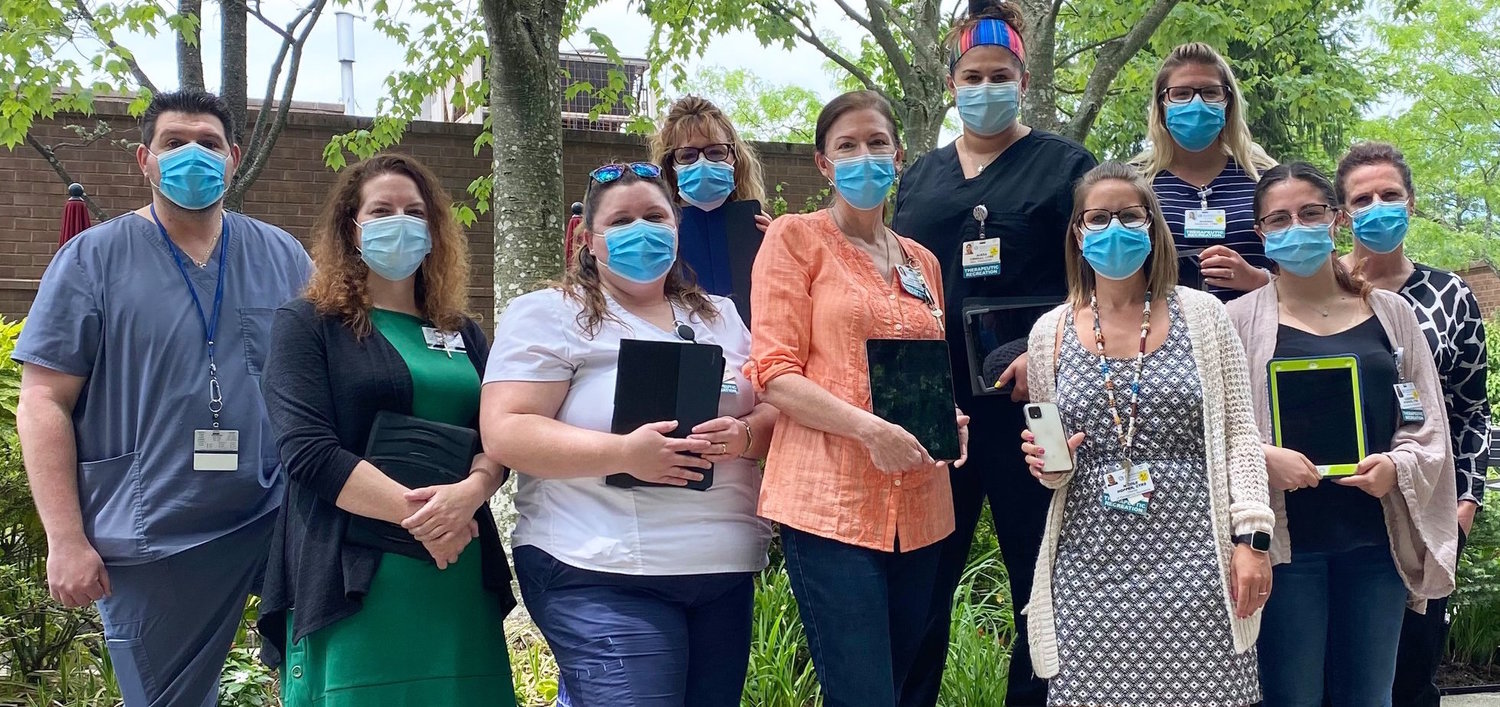
JNS spoke with Jewish nursing-home administrators — including at Gurwin Healthcare Systems in Commack — to hear from those on the front lines about how they have coped and are still coping, in addition to the lessons learned and efforts to protect the elderly going forward.
One decision they noted was a March 25 mandate by the New York State Department of Health requiring nursing homes to accept coronavirus patients considered to be “medically stable” after being discharged from a hospital, unless facilities could demonstrate that they were unprepared to do so. The order did not require these patients to be tested for COVID-19; in fact, it explicitly said not to.
Gov. Andrew Cuomo later rescinded the order, but not before much damage was done, with the virus spreading rapidly among the elderly.
According to figures released last week by state health officials, 6,500 nursing-home residents have died of COVID-19 out of a total 100,000 nursing-home residents in the state’s 613 facilities. Jewish institutions have not escaped devastation.
Stuart Almer, Gurwin’s chief, explained that it stocked up on Personal Protective Equipment (PPE) and created an “isolation unit” in February in anticipation of coronavirus cases.
“We knew [similar infections] had happened in Seattle, so my instruction was, ‘Let’s get as many masks, gowns and gloves as we can’,” recalled Almer. The home also purchased Plexiglass panels to create the COVID-19 isolation unit.
As of March 25, when the health department ordered nursing homes to admit COVID-19-infected elderly from hospitals, Gurwin — a 460-bed nursing home with other facilities — had one COVID-19 infected resident.
Since then, 60 Gurwin residents have died from COVID-19 in its nursing home, and 13 have died in its assisted-living facility. In the nursing home, 150 residents have recovered, and the facility has now reported zero cases of COVID-19.
Of 1,200 staff members, including nurses, health aides, administrators, and janitors, 130 tested positive for COVID-19, and one “beloved member of the housekeeping staff” has died, said Almer.
A disproportionate number of deaths at Gurwin took place among the “dementia population,” said Almer. Despite tremendous effort by Gurwin’s staff, infection spread there partly because “they are more challenging to direct,” noted Almer. “Our staff did all they could. … I’m very proud of them.”
At present, all staff is screened daily upon entrance with temperature checks. Additionally, Gurwin tests every employee weekly for COVID-19.
Almer is thankful to UJA-Federation of New York and the Association of Jewish Aging Services for helping supplement Gurwin’s supply of PPE, and said additional support for more PPE and more testing — the costs of which he describes as “astronomical” — would “go a long way” to help ensure the facility remains COVID-19-free.
Family and friends from outside the facility have been prohibited from visiting residents “for months,” according to Almer, who in solidarity with families didn’t see his 89-year-old father, who lives in the facility, for three months.
Almer said he accepted the March 25 mandate because “we had an isolation unit, and the mandate was clear.” But he added that in the future, nursing homes need better representation in such fast-evolving situations.
In case of a future surge, vacant buildings, including in nearby Suffolk County, could be secured by the state as dedicated COVID-19 treatment facilities, he said.
“There could be a [designated] COVID-positive facility in each county,” he suggested, emphasizing that discussion of the issue is not a matter of blame, but an opportunity for all parties to learn, which he noted is a Jewish value.

 46.0°,
Light Drizzle
46.0°,
Light Drizzle